Pollen has a specific microbiome for every plant species!
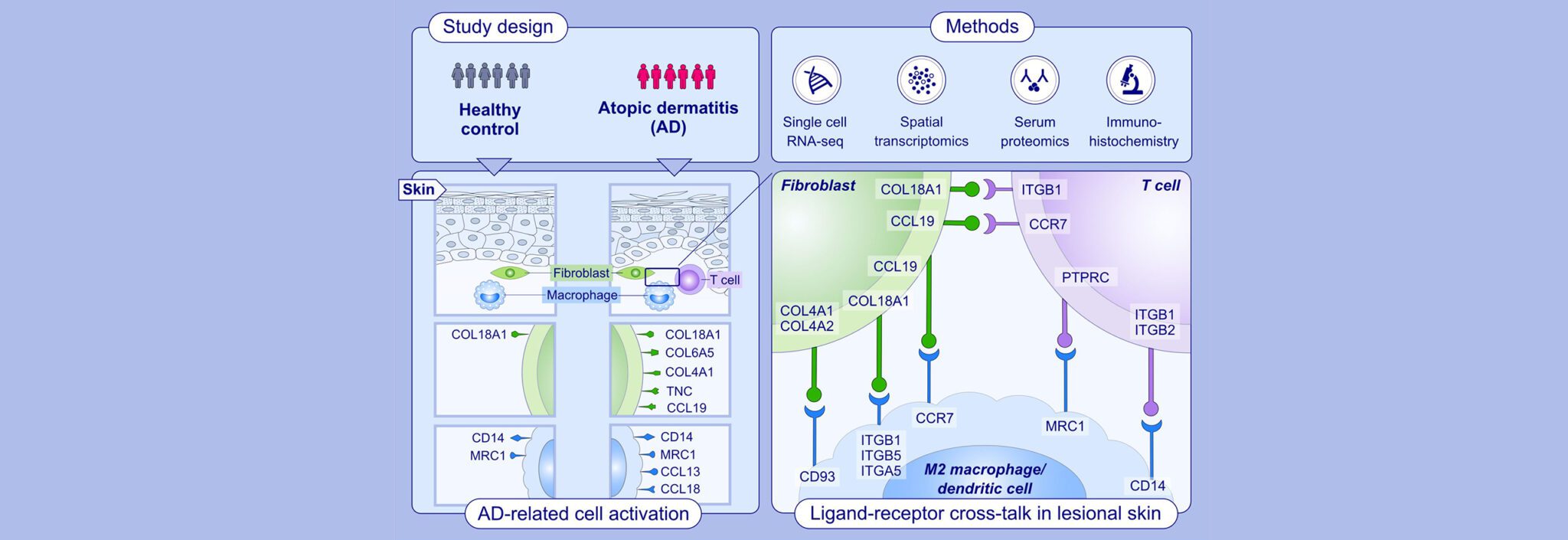
The number and severity of diseases based on pollen allergies is constantly increasing. Scientists now assume that plants’ own defence mechanisms against environmental factors, such as exhaust fumes or adverse microbial overload, bear a significant share of the allergenicity of pollen and pollen-associated compounds. It is important to understand that microbes in themselves do not have a negative impact on plants (and people). Instead, the “right mix” (diversity) of microbes appears to be crucial to the health of human, animal and environment. The publication quoted below first describes the different types and number of microbes to be found on birch and grass pollen. The differences in the pollen microbiome between different species of plant are described as well as the differences between the pollen microbiome of the same plant species, but under the influence of different environmental factors such as location and pollution burden. In a second step, possible correlations between air pollution, pollen microbiome and the allergenicity of pollen were established.
If we damage the environment less, the allergenicity of plant pollen will also decrease
In this connection the research team established that precisely air pollution (traffic load) and a “harmful microbial load” have a negative influence on the allergenicity of pollen – hence more allergen is released. The aim now is to understand what induces pollen to release more allergen and what microbes act as trigger factors in this process. It seems clear that allergen production and allergen release are a defensive reaction – a type of stress situation that is intended to ensure the plant’s survival. A more positive influence on the plant world is needed in future through sustainable management of the environment, so that plants produce less (disease-causing) pollen allergen and hence patients have fewer symptoms and fewer allergies arise.
In February 2016, for the field of medicine, the relevant publication “Pollen-Associated Microbiome Correlates with Pollution Parameters and the Allergenicity of Pollen“ (first author: Andrea Obersteiner) was successfully published in the internationally highly-ranked specialist journal PLOS One. The publication is the result of excellent interdisciplinary cooperation between the Institute for Environmental Medicine at UNIKA-T and the Department of Microbe-Plant Interaction at the Helmholtz Centre in Munich. The scientific colleagues at the Institute for Environmental Medicine, Stefanie Gilles, Isabelle Beck and Franziska Häring, and the Institute Director Claudia Traidl-Hoffmann are pleased that, through their research efforts, they have made a unique contribution to the understanding of the connection between microbiome, air pollution and the allergenicity of pollen.