Scientists from the Swiss Institute of Allergy and Asthma Research (SIAF) in Davos, from the University of Tokyo, the RIKEN Research Institute in Yokohoma, and from Stanford University recently discovered mechanism that stops the body from reacting with an excessive immune reaction. This could be the basis for a new way to handle allergies.
Most people with allergies have to take medication throughout their life: Their body “thinks” that proteins from the environment are so “strange” that they elicit an immune reaction. Until present, it was not possible to develop an efficient therapy so that the body “learns” to stop in an overreacting way.
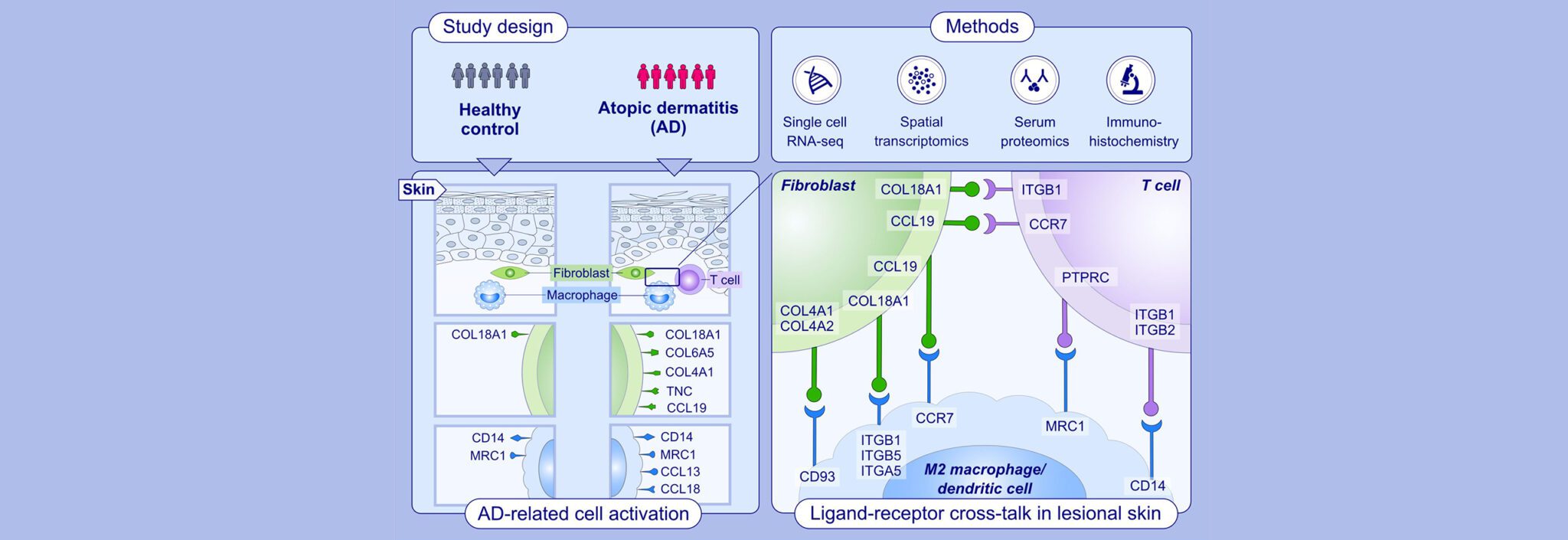
Mast cells play a key role in the disease process in allergies: As a reaction towards an allergen – for example pollen or dust mites – they release big amounts of substances that initiate an inflammatory process. Study leader Hideaki Morita and his team discovered that mast cells are not only “bad guys”, but also have a “good side” (see figure): They release the substance interleukin-2 that induces the production of certain immune cells called T-regulatory (Treg) cells. Treg cells can suppress the allergic inflammatory process in the airways induced by interleukin-10.
It is already known for some time that Treg cells can subdue an excessive immune response and the resulting inflammation. For example, injections with Treg cells prevented autoimmune diseases in mice. However, for Treg cell treatments one needs a large amount of these cells, which is not easy to realise. In the blood, there are just a few of them, and in vitro they are difficult to produce. Using mast cells, Treg cells could be easily produced in the laboratory in large quantities. “The mechanism that we discovered, could be the basis for a new way to handle allergies,” says Hideaki Morita.
Felicitas Witte
Source:
Morita et al., An interleukin-33-Mast Cell-interleukin-2 Axis Suppresses Allergic Inflammation Induced by Papain-Promoting Regulatory T Cell Numbers, Immunity (2015), http://dx.doi.org/10.1016/j.immuni .2015.06.021